Gary Gershony, MD, discusses currently available catheter therapies in the treatment of Structural Heart Disease (SHD).
Dr. Gershony also discusses the prevalence of aortic stenosis in the US, and the unment clinical need for treatment of this disease.
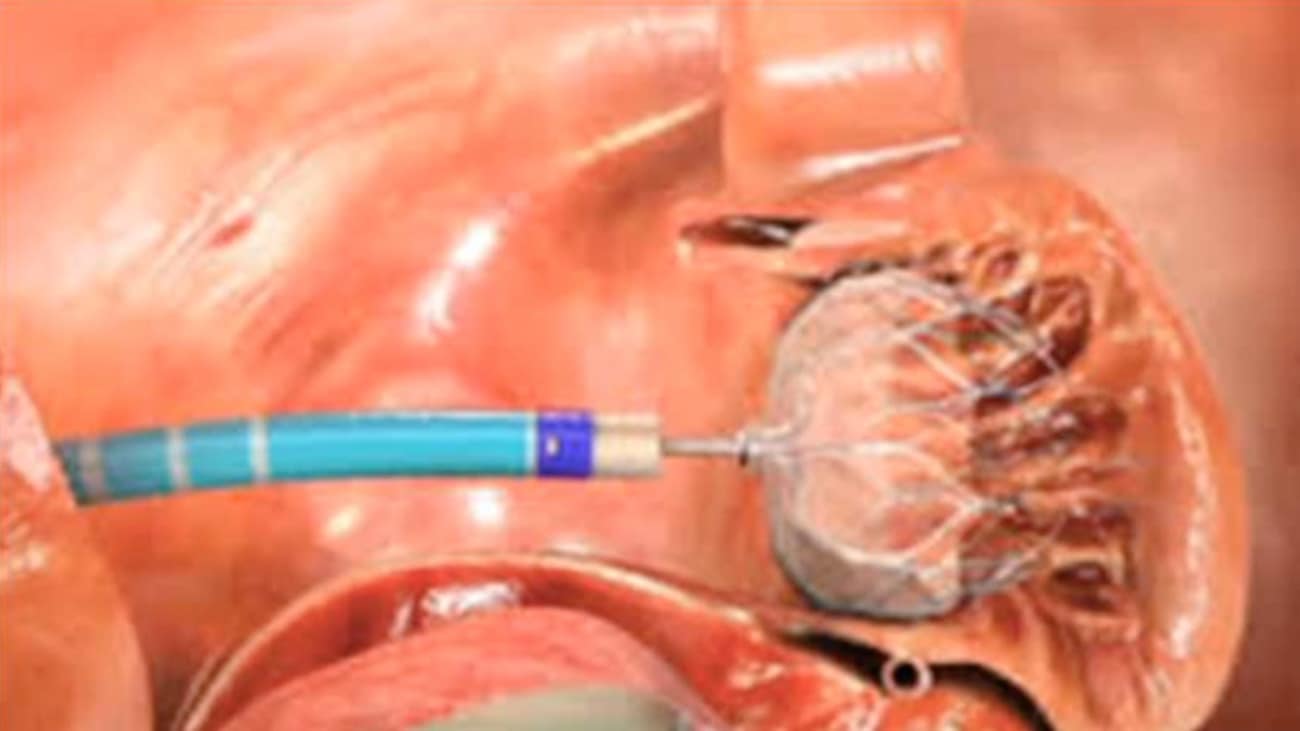
GARY GERSHONY: Good morning, everybody. We'll get started. I'd like to welcome you to our monthly Cardiovascular Grand Rounds. There has been a last minute change. We had a speaker previously arranged, that you may be aware of, to give a talk on diabetes and cardiovascular disease, and because of unforeseen circumstances he did have to cancel at the last minute. I hope that no one minds that we are changing the topic to something somewhat unrelated, but very important in cardiovascular medicine. And programs that are very active at John Muir Health that I think is going to be valuable to update for all of us. My name is Gary Gashony. I'm an Interventional Cardiologist at John Muir Health. And I am Director of cardiovascular research, education, and technology at John Muir Health and in the Cardiovascular Institute. The topic of Grand Rounds today is catheter-based treatment of structural heart disease. So this is a very large and evolving area, and just to give a sense of some of the active areas within cardiovascular medicine, where catheter-based technologies are becoming more and more important, I think that one can divide these up into two broad categories. Acquired adult structural heart disease-- the term SHD as a short form is increasingly being used. And the main areas within acquired adult structural heart disease are aortic valve stenosis, mitral regurgitation, mitral stenosis, prosthetic valve para-valvular regurgitation. That means leakage of valve which had been previously implanted surgically. And left atrial appendage closure for atrial fibrillation also a very important area. And with the recent approval this past week by the FDA of the first such device is going to become increasingly important in the future. And then the second broad category, which I'm not going to spend any time on because it's really a separate discipline, which is adult congenital structural heart disease. And there are many different forms of this disease, and increasingly, patients who have survived into adulthood because of the outstanding work that's been done by the pediatric cardiovascular surgeons, often they need additional revisions. Many of these can be done percutaneously, through catheters. And some of the more common ones that I've listed there-- ASD and PFO closure, VSD closure, and I've also included bicuspid aortic valve stenosis, which is a congenital abnormality, although it's often lumped together with other forms of aortic valve stenosis. Though, with current iterations of catheter-based devices to treat it, still is not optimally being managed because it really is structurally a different type of disease. I'm going to really focus mainly on the acquired forms, and I've highlighted in yellow on the slide the ones that I think are most relevant and most important to our discussion today. So let's talk first about aortic stenosis. There are an estimated-- somewhere in the range of 2% to 9% of US adults over the age of 65 with severe aortic valve stenosis. It really varies based on the studies, and I'll show you some of those in the next slide. The most important ideologies are degenerative calcific, or what we might consider wear and tear, and there's quite a bit of research going on at a basic cellular level to try to understand better why some patients do get this and others do not. It's not clear that it's simply wear and tear. And bicuspid disease, which represents about 30% of these adult patients in the US and other developed countries. Now, there are other ideologies in less developed parts of the world. So rheumatic heart disease still a very important culprit in aortic valve disease elsewhere. But by and large in the US and in Western Europe, rheumatic heart disease become much less common than it used to be in the past. It is still felt that the majority of patients with aortic stenosis are either undiagnosed or undertreated, and there are a number of reasons for that. We also know that this is a very lethal disease, and we sometimes forget that this is as lethal as many malignancies, and certainly as lethal as other forms of cardiovascular disease, including coronary artery disease. And when patients develop symptoms, generally speaking, untreated, the median survival range is in the two to three years. So very lethal disease and something that we need to pay attention to. Often these patients are very elderly, even well beyond being octogenarians which may, in fact, be part of the reason why our treatment tends to be less aggressive. And frequently they have multiple comorbidities. Partly because there's a perceived high mortality, morbidity for conventional surgical AVR, which is often not correct, because in skillful hands, currently, surgical aortic valve replacements has a overall as low or a lower mortality as an isolated procedure to multi-vessel bypass surgery. And that may very well be the most frequent cause of undertreatment because of that misperception. This slide summarize several studies that have been done in the past looking at the prevalence of aortic stenosis. I particularly like the one on the right side from Olmstead County. And some of you may know that that, in fact, is the county in which the Mayo Clinic resides, and they've done a very good job tracking patients there. But if you look at this, you see that by the time patients get into their 70s and beyond, close to 10% of the population have significantly aortic valve stenosis. So it's a very important and growing problem, particularly with the aging population. What about in our own neck of the woods here in Contra Costa County? We know that our own population is aging, and the proportion of patients older than 65 has increased in the last few years and now exceeds 12%, projected to increase up into the 17% range later this decade. And the prevalence of clinically significant aortic valve stenosis will increase within our own population. So what are the types of pathologic entities that we have to deal with with aortic valve stenosis? This slide shows you some good examples. The one that we are primarily focusing on today, in terms of catheter-based technology is the degenerative calcific tricuspid aortic stenosis on the upper far left. And this is generally valves that were normal at birth, and over a period of many years developed fibrosis and thickening of the leaflets and calcitation. Bicuspid aortic valve, which the true form is a congenital variety in which there is, during development a fusion of one of the commissures. There are a variety of subtypes of bicuspid aortic stenosis, and that leads then to one larger leaflet, if you will, and a smaller one. And the [INAUDIBLE] dynamics that result from this type of congenital abnormality leads to premature or early aortic valve stenosis, so that typically patients with bicuspid aortic valve stenosis develop a significant disease when they are in their 50s or younger. Whereas those with degenerative calcific aortic valve stenosis typically present after age 65. We've already talked about rheumatic aortic stenosis which is very uncommon now in the US and Western Europe and developed countries. I think it's very important to remember that the structures and the complex that surrounds the aortic valve has a lot of very important relationships to critical structures. And I think this slide does a very good job summarizing this. This was in a paper by [INAUDIBLE] Piazza, in circulation a number of years ago, and has really stood the test of time. But again, just to remind everyone, when we are dealing with the aortic valve, and particularly when we're trying to treat it remotely with a catheter and be very precise about placement, not positioning it in the optimal location and just being off by several millimeters can have very dire consequences. So when we look here, you can see that the aortic valve itself, of course, originates within the root or the annulus. The coronary ostia are very close so that when it can impact the coronary circulation, the anterior mitral valve leaflet is in close proximity, and so malpositioning of a valve or imprecision in the positioning of the valve can lead to interference [INAUDIBLE] mitral valve. The conduction system resides, or parts of it in the membranous septum, which are in close proximity. So an impact on the conduction system and the need for pacemakers in some patients has been recognized. And then left ventricular outflow track is close by, and so interfering with ventricular mechanics can also result with imprecise positioning of a transcatheter valve. So the first valve that was actually approved in the United States and actually implanted in the world was a variant of the valves that we're now using called the Sapien valve, developed by a company called Edwards Lifesciences. They had acquired a small startup company called Percutaneous Valve Technologies, PVT. And essentially what was designed was a bioprosthetic valve with bovine leaflets, pericardial tissue leaflets, similar to what are used in the surgical bioprosthetic valves that were sutured into a stent-- a balloon expandable stent that you can see here. And this is then crimped on to a balloon of the appropriate size for the annulus, the aortic valve annulus. And the original design that was approved in the US with Sapien was then delivered through a variety of routes, transfemoraling about half the cases. And the catheters were too large, so that the other half, other access sites, including transapical and transaortic were utilized. Here you can see the tranapical approach, and then the balloon is inflated in the annulus. Because of the need for improvements in design and miniaturization, the next generation device, the Sapien XT became available almost a year ago. And there were improvements both in the design of the [INAUDIBLE] and the underlying stent structure. But most importantly, improvements in the catheter delivery system, making it lower profile and more able to deliver the valve successfully. You can see here that additional sizes were added. Originally we had 23 and 26 millimeter. Now there's 29. But even with that, there would be an advantage of having additional sizes to be optimally matched to the patient's annulus. This slide summarizes the differences in terms of the two values, with this going from stainless steel stem to a more robust a cobalt alloy similar to what we use with coronary stenting that are [INAUDIBLE] strength, radial strength inner struts, and then some change in the leaflet geometry to improve durability. So the Sapien XT is now the version that's being used in the US commercially. And this slide just summarizes the improvements in the catheter delivery system. Some very clever design changes were made so that as opposed to the original design where the stent and the valves were crimped on the balloon right at the beginning of the procedure, in efforts to minimize the diameter of the catheter and the delivery system, the stent is actually placed onto the balloon inside the body once the catheter is delivered to the aorta, and that allows for a very significant decrease in the profile of the device. Here you can then see in a more graphic, or in a more clear representation the differences between the original design, the RetroFlex 3 delivery system, 22 french internal diameter versus 18 french on the NovaFlex, and that's resulted in about a 33% reduction in the outside or outer diameter cross-sectional area. Which for a lot of these elderly patients really is a dramatic improvement in terms of our ability to access the femoral artery as the main delivery site, and the avoidance of potential vascular complications. So what led to the original approval of the device in the US was the PARTNER I trial, which was initially reported in the New England Journal of Medicine about five years ago. Here you can see a summary table showing in that randomized trial of the Sapien device, the first generation device, versus surgery in patients at high risk. These were typically patients that had multiple comorbidities and were frail, and had an STS score of over eight. And what this trial shows that for the main endpoints, the transcatheter delivered valve was not inferior to surgery in terms of mortality, one year and at 30 days, and other major outcomes. There was a trend toward a higher rate of stroke, and a lot has been published about this, and a lot of analyses about this. And more recently, and with the next iteration devices, and with improved operator skill and technique, more recent studies have suggested that the stroke rate has actually become comparable between both the transcatheter approach and surgical approaches. So at the present time with the current version of the device and at experienced centers, at least the current data suggests that there is no significant difference in the major [INAUDIBLE] of death and stroke. Importantly, the five-year data from the first PARTNER trial, the PARTNER I trial was just presented at the American College of Cardiology meetings in San Diego. And you can see here that this slide shows the durability out to five years. Of course we want to know even longer than five years. But for these primarily elderly patients at high risk, five-year data is very substantial, and you can see here that the cath and [INAUDIBLE] curves show that out to five years there's really no significant difference in the rate of all-cause mortality and stroke between patients who were treated with the transcatheter approach, versus those that were treated with traditional surgical AVR. This study shows that when you look at the next generation of Sapient device of the XT with the lower profile and some design changes in the catheter, and that effect on vascular complications. If there has been a significant reduction in major complications, including vascular perforation, dissections, with the Sapien XT, with the next generation device, as compared to the first generation Sapien. Clearly, an advantage in improvement with this next generation technology. The other major device that is currently approved in the US for transcatheter aortic valve replacement is the CoreValve device which is currently owned by Medtronic. This is a very different design than the Sapien device. It's a self-expanding nitinol cage, rather than balloon expandable. It is in an 18 french delivery system, which is a similar profile to the current Sapien XT. As opposed to the bovine leaflets that are utilized in the Sapien device. This utilizes porcine-derived pericardial leaflets. And importantly, though not listed on the slide, the actual valve is supra-annular. What that means is that when the device is implanted in the annulus, the leaflets are not there, but they are supra-annular. And that has some advantages and disadvantages that pertain to different anatomic situations. But it is a very different design than the Sapien valve, and it's available in four different sizes. This, too, is an important study that was presented at the American College of Cardiology meetings this past week. And this is now the two-year data from the pivotal trial of the CoreValve in the US. Now, this is a very interesting trial. It's different in many respects to the Sapien trial because it looked at lower risk patients, so the average STS score was lower. And these really represented closer to intermediate risk patients and to high risk patients. And what's quite interesting in this trial is when you look out to two years-- and this was first noted at the one-year follow-up that was presented a year ago at the cardiology meetings. But now even up to two years you can see that the curves continue to diverge, and that all-cause mortality is actually higher in patients treated with surgery, with traditional surgery, than those treated with the transcatheter treatment. So again, to reiterate, that there is a statistically significant difference in the mortality rate at two years between TAVR and surgical AVR with TAVR actually having a statistically significant lower mortality rate at two years than patients treated with traditional surgery. So obviously, these patients need to be followed out for a significantly longer timeframe than two years. But this is intriguing. And of course, the first trial that shows that the transcatheter approach may not just be equivalent, but may, in fact, in terms of certain endpoints of mortality may be safer than traditional surgical approaches. At John Muir Health we have a team that are involved with TAVR. So the heart team approach is very important. In some of these newer complex procedures, it requires the skills of those physicians that have been involved with surgical valve replacement for many years and understand the anatomic considerations better than anyone, and have some unique skill sets. It requires the skill of catheter-based cardiologist or interventional cardiologist. And imaging is extremely important here in terms of guidance and identification of complication. So you can see, because of that there is representation from interventional cardiology, cardiovascular surgery, imaging cardiology, and interventional radiology. And then, of course, all of this needs to be organized and having the skills of valve clinic coordinators to make sure that everything is collected, all the data's collected appropriately, and patients are scheduled safely is in the hands of two very capable coordinators at our own high risk valve clinic. So what about our results at John Muir Health? So these are the results as of November 2014. We had completed 80 procedures. We're now approaching 100, and the volumes are increasing in terms of the number of cases that we're doing quarterly. And I think some of that has to do with skill set, the increasing awareness of the community and identification of patients. But as of November, we had completed 80 procedures, and were successful on deploying a valve in almost all of them, in 99%. As you might expect, these are elderly patients. The average age here is 84 years old. An equivalent number or percentage of men and women, so that's somewhat different than what we see in studies or in registries of other types of cardiovascular disease. Vascular sclerotic disease, this is an equal opportunity disease for men and women. And then you see here that our average STS score was quite high, almost eight. And this really underrepresents the complexity of many of these patients, because the STS score as it's currently designed does not include a lot of important comorbidities that increase the patient's risk. And there's also an important concept called the frailty index. Many of these patients are very frail, particularly because of their age and comorbidities, and that's not captured in the STS score. We felt that [INAUDIBLE] dealing these patients and including them in the National Registry, the TBT Registry that's administered by the ACC and the FDS, that 87% of these patients fit with so-called PARTNER A, very high risk. And 13% of them would have been deemed inoperable, or PARTNER B. As you can see on this slide, these patients had significant comorbidities. About 30% of them had COPD. 15% had had a prior stroke. 43% had had prior intervention for significant coronary artery disease. These are either bypass surgery or PCI. A quarter of them had peripheral vascular disease, and they all had pre-aortic valve stenosis, as shown there. In our early experience, when we had the first generation, which was, of course, the much larger delivery system Sapien, we could only do about half the procedures through a transfemoral access. That is the default, and that is the preferred technique, because the recovering for the patient, and some of the complications that occur with TAVR are less with the transfemoral approach. So it is generally the preferred approach. It's easier on many of these elderly, fragile patients. About half the cases we had to do through a non-transfemoral approach. At the beginning we primarily used transapical, and more recently shifted [INAUDIBLE] transaortic approach, which we think has significant advantages in certain patients. And you can see here, the majority of the valves that we have implanted are Sapien valves. This includes Sapien XT as well. And just the minority, just about 7% or so, were the Medtronic CoreValve. And here you can see when you compare our results, particularly the critical results such as death and stroke both at 30 days and one year, so this is the John Muir Health results. These are the comparator which are the National Registry, the TBT Registry or National Cardiovascular Data Registry administered by the American College of Cardiology and the Society of Thoracic Surgery, that we fair quite favorably. Our 30-day death rate is lower than what is reported nationally. Our rate of stroke is comparable, and the one-year death rate is comparable to what has been published in prior studies in the PARTNER trial. The NCDR has not yet reported on one year death rates because it's a relatively new registry. You can also see that we have a relatively low rate of permanent pacemaker implantation, which is very favorable. And that may also reflect that we have been primarily using the Sapien valve that is known to have a lower requirement for permanent pacemakers than the CoreValve. Our average length of stay for all patients is comparable to the National Registry. And you can see that there's a significant difference between patients that are transfemorally treated, or through transfemoral access as compared to the non-transfemoral approach, so a substantial difference in hospital stay, as you can imagine, because of the greater invasivity. When you do a transapical or transaortic approach it requires either a lateral thoracotomy or a sternotomy. Also very importantly, our results, with respect to para-valvular regurgitation are very favorable. Here you can see that only 8% of patients had moderate or severe para-valvular regurgitation. The importance of this is that it has been shown in a number of studies that not only are patients more symptomatic, if they have residual leakage around the valve where it's not seating optimally, but it also has a very significant impact on mortality at one year and beyond. So the goal with TAVR is to try to achieve the lowest rate or minimal amount of para-valvular regurgitation. And even at this point I think these are quite favorable compared to previously published study results. And most importantly, for many of these elderly patients is not necessarily survival, but their quality of life. These patients are all symptomatic, many who have overt congestive heart failure. And you can see that as compared to baseline, there's a dramatic shift where virtually all the patients have very significant congestive heart failure symptoms at baseline, but at 30 days and one year, the overwhelming majority of them are in either New York Heart Association I or II in terms of symptoms. So a dramatic improvement in symptomatology. What are the current limitations of TAVR? We've already talked about the miniaturization or making the diameter of a sheath and delivery system more favorable for a fully percutaneous transfemerol access. [INAUDIBLE] para-valvular regurgitation because of its impact on survival and also symptoms, so diminishing the incidence and making it as trivial as possible. Some of the problems with positioning the valve and if we're in the wrong place, how are we able to reposition it? Current generation devices that are commercially available do not allow for easy repositioning if it's necessary. Device embolization tends to be very rare, particularly with the Sapien device. Perhaps a little more common with the CoreValve. Embolic CVA and TIA, if we can reduce this to near zero that would be a very important advance. And then the need in a pacemaker on patient post-procedure that is more frequent with the CoreValve than with the Sapien valve. So why is para-valvular leak so important? Why do we care so much? It's certainly much more than a cosmetic problem. Here you can see in the study, looking at the PARTNER trial data that out to three years, continuing divergent to the curve based on patients who had minimal, none, or traced the order regurgitation. So this is their all-cause mortality as compared to those with mild or severe, and the curves are continuing to diverge out to three years, and this was highly statistically significant. This is corroborated in a number of other studies and registries. So we know that it is important to minimize the degree of para-valvular regurgitation. So this slide shows a number of technologies are meant to improve outcomes in the future, or at least hope to improve outcomes. On the upper left, you can see there the S3 or the Sapient 3. This is the next generation of Sapien valve that has been studied both in the US and internationally. Data with the S3 was just presented to the American College of Cardiology and the specific design here has a cusp around the annular region to minimize leakage around the valve. And also it's a lower delivery system, 14 french, which will be suitable for a significantly larger percentage of patients so that this can be done percutaneously and less invasively. And the data that was presented at ACC indeed did corroborate [INAUDIBLE] historical data, this valve does appear to be associated with a significantly lower rate of para-valvular regurgitation, and a lower rate of vascular complications. And there's a series of other valves here with different designs. Most of these are self-expanding, actually. Nitinol cages with different leaflet designs. So the next area of improving the transcatheter aortic valve replacement is to minimize the rate of embolic complications, primarily CBAs and strokes. Some of that is operator and technique dependent. We know that if we are very careful with how we deploy the valve, we avoid injury to the aorta, particularly the aortic root, and the aortic arch where there may be friable material if we minimize the number of balloon inflations. These seem to be at least operator dependent techniques that can minimize it. But yet, even with very experienced programs and with the most current generation devices, there's still a major stroke that is in the 2% range, comparable to, perhaps, what one gets with surgical aortic valve replacement. But it is a very devastating complication, and to the extent that we can reduce it even further, that would be important. So these are, in fact, three different devices that are currently being studied to lower the rate of embolic stroke during the TAVR. And two of them have been reported recently. The-- oops. Sorry. The Montage device by Claret Medical was recently published and showed a significant reduction in the number of targets on a diffusion-weighted MRI, suggesting a lower embolic burden to the brain, as compared to the control group. And this TriGuard device was just reported at the American College of Cardiology meetings in San Diego in DEFLECT III trial, and yet again, showed a significant reduction in the MRI targets in the brain with the TriGuard device, as compared to the control group. And there was also, though a relatively small study, was empowered to look at clinical outcomes, there was a trend towards improvements in the cognitive function, in other neurologic function in the patients that were treated with the TriGuard device as compared to no embolic protector. So I think that these devices, particularly in patients that we may deem to be at higher risk for stroke will become important adjunct treatments. None of them are yet approved in the US. This is an example of the Embrella device, which is actually owned by Edwards and which is in clinical trials, and it is essentially a nitinol structure with a filtering device that's placed in the aortic arch, and acts as a umbrella, if you will, to filter away any embolic material. This is the Claret Medical device, or the Montage that was reported last year. The clinical trial showed a significant reduction in embolic targets in the brain on diffusion-weighted MRI. How this device works is these small wind socks, if you will, are placed in each carotid artery percutaneously, generally through a transradial approach as an adjunct during the TAVR procedure. And this finally is the TriGuard device, which was, as I mentioned, just reported in the DEFLECT III trial at the American College of Cardiology meeting. And it's just a different type of embolic protector with, again, a unique nitinol type of structure-- self-expanding. A positioning structure to make sure that it sits in the proper location and protects the major arch vessels, the vertebral and carotid arteries bilaterally. I'm going to shift gears now to mitral valve disease, and so as opposed to the aortic valve where aortic stenosis is the primary pathologic entity, which we are currently treating with transcatheter techniques. In the case of the mitral valve, the main pathology is actually regurgitation or leakage valve, not stenosis. Mitral valve stenosis has become a relatively rare problem in the US and in developed countries because that's primarily been a disease of a rheumatic type of heart disease, which is quite uncommon now. But mitral regurgitation is a very common structural heart disease. Pathology generally comes in two different variants I'll talk about in a moment. I'm oversimplifying it, but it's so-called functional or secondary mitral regurgitation, and a degenerative type or primary mitral regurgitation, which actually primarily affects the leaflets in the valve structure itself. Whereas secondary or functional mitral regurgitation is generally a disease that occurs because of underlying disease in the left ventricle, which secondarily causes the mitral valve to not collapse properly. So how common is mitral valve disease? Well, I mean if you look at these slides, this is even a bigger problem perhaps than aortic valve stenosis. And here you can see this type of studies, either population-based studies or another study that was conducted, again, by the Mayo Clinic in Olmstead County. But by the time that you get into your 70s, you're looking at rates that are approaching 10% with significant mitral valve disease. And it looks like in some of these studies that it is actually more common, the aortic valve disease. This graph here, the aortic valve is the green line, and the mitral valve is the yellow line. And in both of these studies there appears to be a higher incidence as we age of mitral valve disease. This slide shows the mechanism by which the first approved device in the US for transcatheter treatment of mitral valve disease works. It's currently approved only for degenerative or primary mitral valve disease. And generally, when we talk about [INAUDIBLE], that includes patients who have different types of mitral valve prolapse, particularly prolapse of the P2 scallop of the mitral valve. And you can see here, the device that is delivered trans-interatrial septum through the mitral valve leaflets under Echo guidance, and clips the leaflets together in the middle. And this is meant to simulate the well-known Alfieri stitch or Alfieri procedure. Alfieri is a cardiovascular surgeon in Milan, Italy and he pioneered this approach, where in higher risk patients, placing a stitch between the two leaflets was a way to create this double orifice, which reduced the total amount of mitral regurgitation without inducing a significant amount of mitral stenosis. Now, that procedure, the surgical approach, has been superseded by better approaches, more effective, the durable approaches for reducing mitral regurgitation with mitral valve repair. But it has lended itself, at least the Alfieri type procedure has limited itself to the first generation or first approach for mitral valve repair. Here you can see the MitraClip fluoroscopy being delivered. So it's through a trans-interatrial septal approach. And then the clip is passed through the mitral orifice, and here you see under Echo control, the Echo-dense catheter, the two clips, or the two arms of the clip I should say. And here you see the clip being deployed under Echo guidance. So important trial that lead to approval of the MitraClip device in the US with the EVEREST series of trial, particularly the EVEREST II trial was the pivotal trial. And it's already been reported. Here is some of the data that was published in the New England Journal of Medicine recently. And baseline characteristics in this randomized trial that compared the MitraClip for percutaneous repair versus surgical repair of the valve. And you can see that these patients that were randomized two to one had very similar baseline characteristics. And then for the primary Epic CN point listed here, the device was shown to be non-inferior in a composite endpoint that included both the efficacy, as well as major adverse events. But if one looks specifically at efficacy, you can see here that the ability to reduce the mitral regurgitation was definitely superior with surgery. So patients that needed to have surgery for mitral valve dysfunction on follow-up was much lower in the surgery patient than it was in the percutaneous repair patients, and highly statistically significant. And if you look at adverse events, on the other hand, this is where the percutaneous approach did better than mitral surgery, traditional mitral surgery. And this was, interestingly enough, even though you can see here that overall, major adverse events at 30 days were much lower with the percutaneous approach than surgery, highly statistically significant. This was primarily driven by the requirement by a lesser requirement for blood transfusion in the percutaneous group as compared to surgery. So the upshot of all of this is that it was felt reasonable to approve this device for patients who have highly symptomatic mitral regurgitation who are not good surgical candidates. But with the understanding that this technology is still not an ideal way to repair the valve, but it is our first entry into transcatheter repair of mitral valves. Similar to the situation with transcatheter aortic valve replacement, a MitraClip or mitral valve repair team was put together. And again, the surgical skills are critical here. Catheter-based skills, the intervention cardiologist and imaging is even more important here than TAVR. So you can see representation from all the major disciplines on this team. I think that we're getting very close to our first procedure, and a lot of preparation in terms of identifying a first group of suitable patients for the procedure. I'm going to finish off here with left atrial appendage closure, which has become even more important with the recent approval last week by the FDA of the first device specifically for left atrial appendage closure, the Watchman device. And it's the best studied of the three devices I have listed here for left atrial appendage closure. So the Watchman device was studied in two randomized trials, PROTECT AF and PREVAIL trials, and on the basis of those trials, the FDA finally decided to approve it. It's been a long haul. The Amplatzer Cardiac Plug is another catheter-based approach for left atrial appendage closure. It's still in clinical trials. And finally, the Lariat device which has 510k clearance, but it's not specifically approved for left atrial appendage closure, but it works in an entirely different way. It's meant to simulate the surgical approach for left atrial appendage exclusion by placing a snare around the left atrial appendage through catheter-based techniques. It is available, however, the FDA has recently rolled back approval of this device, or at least the marketing of it with the requirement for additional studies, because it wasn't initially approved specifically for left atrial appendage closure through the 510k pathway, rather than through the so-called PMA pathway. So the trial that finally led to approval of the Watchman device was the PREVAIL trial. This was presented at last year's American College of Cardiology meetings, and has been published now in the Journal of American College of Cardiology last year. And it was a prospective randomized trial comparing the Watchman device, which is a catheter-based device for closing the left atrial appendage, and comparing that to warfarin therapy in patients with atrial fibrillation. So the notion here is that it is believed that the majority of clots and embolic material that originated in the heart in patients with atrial fibrillation and lead to embolic complications, primarily strokes, the majority of those originate in the left atrial appendage. And if you can effectively exclude the left atrial appendage through a percutaneous catheter-based technique, that you might be able to achieve at least comparable results to warfarin. And indeed, the PREVAIL trial did show that overall, the rate of life-threatening and major strokes were reduced with this device, and as a result, the device is not inferior to chronic warfarin therapy. And the advantages are, of course, that the patients don't have to take lifelong warfarin and have the bleeding complications. The original study, the PROTECT AF did show a trend towards higher procedural complications, and because of that, the FDA required the second trial be done, the PREVAIL trial. But now on the basis of both of these trials, the FDA felt it was appropriate to now approve this device. This is, in fact, what the Watchman device looks like. It has a nitinol cage or nitinol structure with fabric around the outer aspect of it. And then there are some very small hooks that are not visible in this picture. And under Echo cardiographic guidance, which is crucial for delivery here, this device is delivered percutaneously through a catheter, delivered initially from the femoral vein through the interatrial septum, and then positioned at the orifice or os of the left atrial appendage to occlude it. So summarizing the prior discussions that we've had today, I think that it's clear that the incidence and prevalence of structural heart disease is increasing with an aging population, and particularly also with the improved survival of patients with adult congenital heart disease. And catheter-based therapy for structural heart disease is one of the most rapidly advancing areas in cardiovascular medicine. It is likely that this type of approach, catheter-based treatment of these diseases will become the dominant treatment for many, if not most, adult patients with structural heart disease in the next five to 10 years. And multiple studies are being conducted in the US and elsewhere to confirm that this is the correct approach to treating many of these patients. Current development efforts are focused on improving the results and reducing the complications associated with transcatheter aortic valve replacement, as well as developing more effective devices for the treatment of mitral regurgitation. Thank you for your attention.